Bi-PAP is a mode of respiratory ventilation used in the treatment of sleep apnea. PAP ventilation is also commonly used for those who are critically ill in hospital with respiratory failure, in newborn infants (neonates), and for the prevention and treatment of atelectasis in patients with difficulty taking deep breaths. In these patients, PAP ventilation can prevent the need for tracheal intubation, or allow earlier extubation. Sometimes patients with neuromuscular diseases use this variety of ventilation as well. CPAP is an acronym for “continuous positive airway pressure“, which was developed by Dr. George Gregory and colleagues in the neonatal intensive care unit at the University of California, San Francisco.[1] A variation of the PAP system was developed by Professor Colin Sullivan at Royal Prince Alfred Hospital in Sydney, Australia, in 1981.
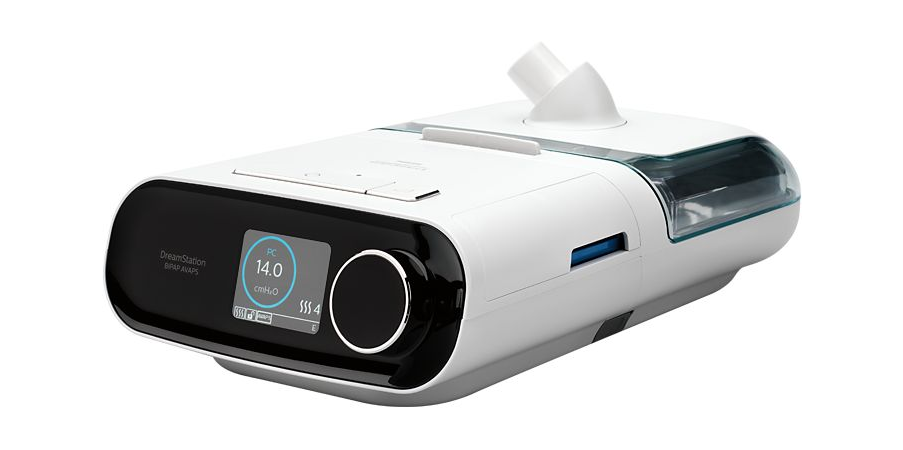
Every patient suffering from chronic respiratory disease has changing therapeutic demands. With DreamStation BiPAP AVAPS noninvasive ventilation solutions, you have the power to treat them that way. Using clinically proven therapy solutions, DreamStation noninvasive ventilators adapt to these changing patient needs, helping to normalize ventilation.
Meeting unique patient needs
Custom and connected care
Clinically proven solutions
Patient driven design
The main indications for positive airway pressure are congestive heart failure and chronic obstructive pulmonary disease. There is some evidence of benefit for those with hypoxia and community acquired pneumonia.[3]
PAP ventilation is often used for patients who have acute type 1 or 2 respiratory failure. Usually PAP ventilation will be reserved for the subset of patients for whom oxygen delivered via a face mask is deemed insufficient or deleterious to health (see CO2retention). Usually, patients on PAP ventilation will be closely monitored in an intensive care unit, high dependency unit, coronary care unit or specialist respiratory unit.
The most common conditions for which PAP ventilation is used in hospital are congestive cardiac failure and acute exacerbation of obstructive airway disease, most notably exacerbations of COPD and asthma. It is not used in cases where the airway may be compromised, or consciousness is impaired. CPAP is also used to assist premature babies with breathing in the NICU setting.
The mask required to deliver CPAP must have an effective seal, and be held on very securely. The “nasal pillow” mask maintains its seal by being inserted slightly into the nostrils and being held in place by various straps around the head. Some full-face masks “float” on the face like a hover-craft, with thin, soft, flexible “curtains” ensuring less skin abrasion, and the possibility of coughing and yawning. Some people may find wearing a CPAP mask uncomfortable or constricting: eyeglass wearers and bearded men may prefer the nasal-pillow type of mask.
Breathing out against the positive pressure resistance (the expiratory positive airway pressure component, or EPAP) may also feel unpleasant to some patients. These factors lead to inability to continue treatment due to patient intolerance in about 20% of cases where it is initiated.[4] Some machines have pressure relief technologies that makes sleep therapy more comfortable by reducing pressure at the beginning of exhalation and returning to therapeutic pressure just before inhalation. The level of pressure relief is varied based on the patient’s expiratory flow, making breathing out against the pressure less difficult.[5] Those who suffer an anxiety disorder or claustrophobia[6] are less likely to tolerate PAP treatment. Sometimes medication will be given to assist with the anxiety caused by PAP ventilation.





Reviews
There are no reviews yet.